Empirical clinical evidence as well as many studies to date indicate that gut health and hormones are closely linked. In particular, recent research shows that the composition and diversity of the gut microbiome play a big role in hormone regulation, especially regarding the key female hormone estrogen.
The studies suggest that poor gut health increases the risk of both excess estrogen and deficiency related conditions including endometriosis, uterine fibroids, breast cancer, PCOS or weight gain.
Therefore, correcting gut dysbiosis (bacterial imbalances in the gut) is considered of key importance by many natural therapists in order to prevent and reverse estrogen-related conditions.
In this post, I’ll discuss and explain why balancing the microbiome could be a key step in preventing and reversing both, estrogen excess and deficiency and related conditions.
Table of contents
- Microbiome regulates hormones and body functions
- How the gut microbes regulate estrogen levels
- Overview of estrogen circulation pathways and metabolism
- Gut bacteria imbalances (dysbiosis) are linked with estrogen imbalances
- Estrogen excess conditions
- Estrogen deficiency conditions
- Estrogen and the integrity of the gut wall
- Estrogen and inflammation
- Gut health, hormones and food intolerances
- Stress, gut health and hormones
- Conclusion
Microbiome regulates hormones and body functions
We know from research that the gut microbiome (comprising all gut microorganisms) regulates many functions including digestion, immune, endocrine and nervous systems. Recent studies show that the gut microbes also play a crucial role in regulating estrogen levels in the body. Therefore, also affecting the levels and ratios of other reproductive hormones linked to estrogen such as progesterone and testosterone.
According to the present understanding, the gut microbiota influences the following hormones:
- Estrogen and other hormones that are linked to its levels
- Thyroid hormones
- Adrenal hormones – cortisol, adrenaline, noradrenaline
- Melatonin (regulates sleep)
Many aspects of gut health can be linked to most disorders known today. My clinical experience dealing with both gut health and hormone imbalances strongly suggests important links between the two, and now research also shows that these links do exist. Therefore in my view, balancing the microbiome is, in many cases, an effective way to prevent and/or reverse most estrogen-related imbalances and conditions.
How the gut microbes regulate estrogen levels
Unfortunately, microbiome imbalances are very common these days. These can be impacted by many different factors such as poor diet, alcohol intake, medications, obesity, age, environmental pollution, plus many lifestyle factors such as high stress and poor sleep, among others.
Common signs of an unhealthy gut include – digestive issues such as bloating, constipation, diarrhoea, reflux, but also chronic fatigue, skin conditions (eczema, psoriasis), weight gain, memory lapses, brain fog etc. Importantly, many symptoms that are seemingly non-gut related are often misinterpreted and either not addressed or mistreated.
We now know that there is a specialised group of bacteria inthe microbiome, called ESTROBOLOME, that metabolise (process and breakdown) estrogens (there are a few types of estrogen).
The gut microbes in the estrobolome regulate estrogens through secretion of an enzyme called beta-glucuronidase that deconjugates (splits) estrogen into its active forms, enabling it to bind to estrogen receptors anywhere in the body. Only the unbound, free estrogen is biologically active.
When the gut microbiome is healthy, the estrobolome produces just the right amount of beta-glucuronidase to keep estrogen in balance. However, when there is gut dysbiosis (i.e. bacterial imbalances), beta-glucuronidase activity may be altered. This activity results in either a deficiency or an excess of free estrogen, thus promoting the development of estrogen-related conditions.
Overview of estrogen circulation pathways and metabolism
Before we continue, I think it’ll be helpful to give you a short overview of estrogen pathways. In pre-menopausal women, estrogen is made primarily by the ovaries (around 90%) and excreted to the blood. It then circulates in the blood travelling to the uterus, breasts and other organs and tissues to perform a number of important functions.
Finally, it reaches the liver where it’s inactivated (conjugated) using specific detox pathways. These are: hydroxylation in Phase I detox and methylation and glucuronidation pathways in Phase II. Good liver function is very important because estrogen that is not properly metabolised by the liver can turn into a more toxic and inflammatory form negatively impacting many body tissues.
The inactivated estrogen is then sent to the intestines where it should stay inactivated so it can be excreted by the body through the stool. So, in the healthy estrogen metabolism MOST of the conjugated estrogen is excreted in the stool and SOME of it recirculates to the body from the gut.
However, when there is gut dysbiosis, the estrogen metabolism is impaired resulting in an overgrowth of a group of bacteria that make beta-glucuronidase enzyme. As mentioned above, when in excess, this enzymere-activates (deconjugates/splits) estrogen in the gut before it can be excreted. So, instead of being expelled, the re-activated estrogen re-enters the body resulting in more than needed estrogen levels. In this case SOME estrogen leaves the body but MOST of it goes back to the body and re-circulates.
Figure 1 displays the known estrogen-microbiome interactions that have effects on the body, according to the current research.
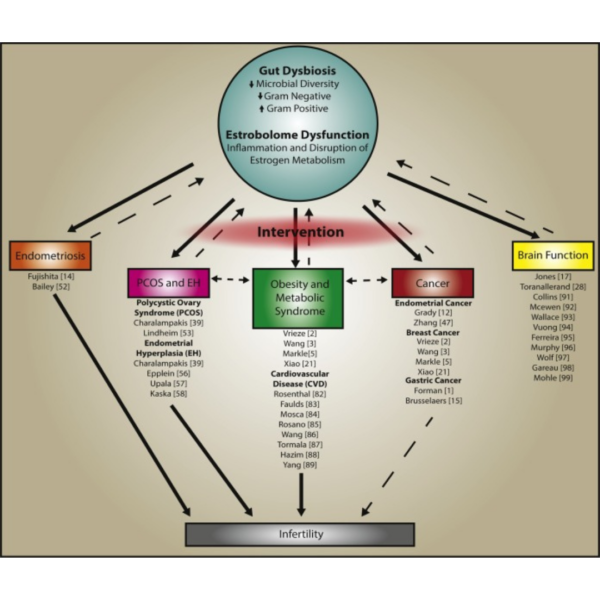
Solid arrows indicate the established interaction between estrobolome and disease states; dashed arrows indicate reputed feedback mechanisms or interactions. View larger image.
As illustrated in Figure 1, many tissues and organs have estrogen receptors, including intestines, brain, bone and fat tissues. Therefore, estrogen has been shown to influence a variety of physiological responses including neural development, cardiovascular health, bone density and cancers.
Gut bacteria imbalances (dysbiosis) are linked with estrogen imbalances
Estrogen plays many vital roles in the human body influencing:
- Female reproductive function
- Regulation of body fat stores
- Cardiovascular health
- Brain function
- Bone turnover/ density
- Cell replication
- Electrolyte balance
- And many more
As stated above, gut dysbiosis has the potential to alter the estrobolome, disrupt estrogen balance and ratios with other hormones. This results in impairment of physiological processes, promoting the development of many chronic diseases.
Main factors include:
- Nutrition status
- Stress levels
- Sleep quality
- Taking antibiotics and other medications – they alter gut microbiome and may cause significant long-term imbalances
- Hormonal contraceptives have been found to alter both the gut microbiota and estrogen levels within the body, suggesting that they may have an adverse impact on the estrobolome.
Estrogen excess conditions
“Estrogen dominance” or excess is a term used to describe an imbalanced, excessively high ratio of estrogen to progesterone. High estrogen conditions can be exacerbated by the out of balance estrobolome with larger numbers of beta-glucuronidase-producing bacteria, leading to increased levels of circulating estrogen. This can exacerbate the following conditions:
Endometriosis
Endometriosis, characterised by the growth of endometrial tissue outside the uterus, has been associated with gut dysbiosis. To learn more, check out this very interesting 2019 study: ‘Endometriosis and microbiome – a systemic review’.
Cancers: Breast, Endometrial, Cervical and Ovarian Cancer
In recent years, studies have linked gut dysbiosis with various forms of cancer. Researchers have found that cancer patients have a significantly altered gut bacteria compared to healthy controls. The altered gut microbiota of cancer patients may lead to increased beta-glucuronidase activity leading to increased levels of circulating estrogen, which binds to estrogen receptors and promotes cell proliferation in estrogen-sensitive tissues.
The microbial balance in the gut may also affect the microbiome of distant estrogen-sensitive tissues, such as the breasts, through direct translocation of microbes into these tissues.
Prostate Cancer
Estrogen is typically associated with women, but men also need it in just the right amounts to be healthy. Low estrogen levels in men, for example, can cause depression, chronic joint pain or weight gain. Dysbiosis of the prostate gland has been associated with prostate cancer, and researchers hypothesise that the gut microbiota may also be markedly different in men with prostate cancer.
Furthermore, elevated estrogen levels have been implicated in the development of prostate cancer, providing further support for the hypothesis that the estrobolome plays an important role in prostate cancer development.
Estrogen deficiency conditions
As stated above, dysbiosis and a reduction of gut microbiota diversity impacts the estrobolome. Reduction in gut microbiome diversity as s result of dysbiosis and inflammation reduces the beta-glucuronidase activity. This reduced beta-glucuronidase activity results in decreased deconjugation/ splitting of estrogen in the gut into its circulating and active forms.
The subsequent decrease in circulating estrogens alters estrogen receptor activations which may lead to the low estrogen conditions such as obesity, cardiovascular disease, metabolic syndrome, and cognitive decline.
Obesity, Heart disease and Osteoporosis
Lack of estrogen and changes in the gut microbiota in postmenopausal women leading to estrobolome disruption is associated with an increased risk of weight gain/obesity, cardiovascular disease and osteoporosis. We know that estrogen also regulates glucose and fat metabolism and bone formation.
Research indicates that the natural reductions in estrogen that occur at menopause impair these estrogen-dependent processes triggering weight gain/obesity, cardiovascular disease, and osteoporosis. Moreover, gut dysbiosis resulting in decreased beta-glucuronidase activity may exacerbate the low-estrogen state in postmenopausal women, further increasing the risk of these chronic diseases.
PCOS
Polycystic ovary syndrome (PCOS) may also be influenced by estrobolome imbalances. Women with PCOS have an excess of androgens in relation to estrogen, as well as an altered microbiome.
Researchers theorise that the altered gut microbiota in many PCOS women may promote increased androgen synthesis and decreased estrogen levels through lowered beta-glucuronidase activity.
Estrogen and the integrity of the gut wall
Gut wall integrity has been shown to be influenced by dysbiosis through the reduction in cell-to-cell junctions (connections) leading to increased permeability (i.e. leaky gut). Subsequently, dysbiotic bacteria as well as undigested food can get to the blood stream. This can lead to local or systemic inflammation and multiple food intolerances, causing the exacerbation or increased risk of disease.
Sufficient estrogen levels are needed to form the inner layer of the gut wall and keep it healthy and tight to retain the contents of the gut inside the wall. Good gut wall integrity is critical to good metabolic health because any changes to intestinal permeability, (i.e. leaky gut), can lead to the development of food sensitivities, fat tissue inflammation (impairing weight control) and autoimmune diseases.
Estrogen and inflammation
Estrogen also helps to decrease various bacterial pathogens and reduces lipopolysaccharide (LPS) induced inflammation. LPS, produced by Gram-negative bacteria, can damage the lining of the gut, cross to the blood and circulate in the body, provoking a strong inflammatory immune response. Estrogen’s anti-parasitic function is yet another example of itestrogen’s protective functions on the gut.
Also, women need sufficient estrogen to regenerate the gut lining, keep inflammation in check and help the brain communicate with the gut. Estradiol, the most active form of estrogen, is necessary for keeping the lining of the small intestine healthy and able to regenerate, keeping gut inflammation levels low. I find that balancing hormones definitely helps with dealing with SIBO (small intestine bacterial overgrowth)!
Gut health, hormones and food intolerances
Hormones affect inflammation and immune tolerance of foods (food sensitivities) we eat because immune cells have receptors to hormones. That’s why hormone fluctuations in women (PMS, perimenopause, etc.) can cause inflammation when the immune system reacts to foods.
Many women who struggle with hormone imbalances also have poor immune function, higher levels of inflammation and many food intolerances This indicates that their immune system has lost the ability to appropriately tolerate the foods they eat. As a result, the immune system starts to react to many foods or ‘everything’ in some cases causing major digestive and absorption problems.
Stress, gut health and hormones
Elevated cortisol produced by the adrenal glands in response to excess stress has a detrimental effect on the intestinal lining integrity (it exacerbates leaky gut), and also suppresses immune sIgA cells that are part of the the immune response in the gut. Both factors contribute to estrogen imbalances by decreasing the number of receptors in the gut or desensitising them. Development of food intolerances, leads to increased inflammation levels that affect estrogen receptors throughout the body.
Conclusion
There are many causes of hormone imbalances, and gut health and changes in your microbiome are not the only way your hormones get out of balance. However, as the microbiome has such a significant impact on your hormones and disease processes in the body, improving your gut health should be a high priority in any therapies, and an excellent starting point.
The good news is you can start improving your gut health and hormone imbalance with your next meal! There is no doubt that nutrition plays a vital role in influencing microbiome composition and diversity. Providing, of course, that you eat foods that are ‘good for you’ but it’s a topic for another post!
Feel free to get in touch if you’d like help with finding the right foods to eat for you at present to start recovering your gut health and balance hormones. Here is a sample of a gluten free and dairy free delicious banana bread recipe you can enjoy that is also good for gut health and digestion.
For convenience and easier access, I offer either Zoom or telephone consultations for Australia-based individuals only. I’m afraid I’m not able to offer any specific advice to individuals based in other countries at this time.
To book a consultation, click the button below. I also offer a free 15-minute initial discussion to talk about your circumstances and how I can help.
I look forward to connecting with you and to helping you to feel healthier and happier soon!
Best of Health
Joanna Sochan
Wholistic Health and Lifestyle Therapist
Natural and Lifestyle Therapies for Abundant Health and Wellbeing
Additional resources
- What is leaky gut? Causes symptoms, remedies
- IgG food sensitivities: testing and clinical applications
- Parasite treatment considerations: Blastocystis and dientamoeba fragilis
- Online naturopathic and nutrition consultations Australia
Disclaimer: The above material is for informational and educational purposes only. It should not be used to self-diagnose and it is not a substitute for a medical advice, diagnosis, treatment, prescription or recommendation. All viewers of this content, especially those taking prescription or over-the-counter medications, should not make any changes in their health regimen or diet before first consulting a doctor or other qualified health provider with any questions they may have regarding a medical condition or their particular circumstances.

Joanna Sochan is a Natural Therapist and founder of Naturimedica Holistic Wellcare. She has a passion for helping clients transform their lives by becoming healthy and well naturally. Joanna has 12+ years experience in clinical practice and has special interest in solving complex cases, gut health, food sensitivities, hormone imbalances, autoimmune disorders and weight loss. She helps clients individually (mostly online) Australia-wide and also offers online therapeutic programs, eCourses and self-help eBooks. View full bio.
 Print This Post
Print This Post 


Leave A Comment