When working with clients who suffer from various stages of adrenal fatigue or burnout, we start by performing adrenal and other tests to help with adrenal function assessment and determining optimal treatment options.
Hence I’m often asked questions about the best testing methods, especially the reasons why I use the saliva adrenal hormones test (measuring adrenal hormones cortisol and DHEA) vs blood or urine testing.
To answer some of these questions I wrote this blog to provide you with an overview of the adrenal function testing options currently used.
Adrenal fatigue or the hypothalamus-pituitary-adrenal (HPA) axis dysfunction is often called the 21st century syndrome being the consequence of the stress related to busyness of our daily lives, lack of sufficient sleep and perpetual juggling of tasks both at work and home.
These stresses accumulate over time and then manifest in many physiological and psychological imbalances that can lead to significant negative health effects, if experienced over a prolonged period of time.
Symptoms of adrenal fatigue
They include physical and/or mental fatigue (often debilitating), sleep disturbances, low energy in the morning and/or during the day, difficulty in concentrating or focusing (brain fog), mood disorders (anxiety, depression, lack of joy in life), many digestive problems, blood sugar imbalances (weight gain, anxiety, heart palpitations and sleep difficulties), immune system impairment and many more.
Check out my post on adrenal fatigue for more details.
When embarking on any treatment of adrenal fatigue, it’s very important to assess the adrenal function by measuring the 24-hour cortisol (circadian/ diurnal) levels which will determine your individual cortisol pattern to gauge how well your HPA axis is working.
This will help to select the right supplements and doses, needed nutrition improvements, and what lifestyle adjustments are required (these are the key to short- and long-term recovery).
In addition to cortisol, another adrenal hormone called DHEA (Dehydroepiandrosterone) is also measured in the saliva adrenal hormones test to further determine a degree of adrenal dysfunction (both readings are needed to assess adrenal function).
As opposed to cortisol, DHEA can be measured at any time of the day. Please note than this important hormone is not discussed in this post, look for a dedicated post about DHEA in the future!
Cortisol 101
Cortisol is the major hormone managed by the HPA axis. Secretion of cortisol by the adrenal glands is tightly regulated and involves:
- Neurons in the hypothalamus synthesise and secrete corticotropin-releasing hormone (CRH)
- CRH acts on the pituitary gland causing the release of ACTH (adrenocorticotropic) hormone
- ACTH travels in blood to the adrenal glands where it stimulates the secretion of glucocorticoid hormones, the main one being cortisol
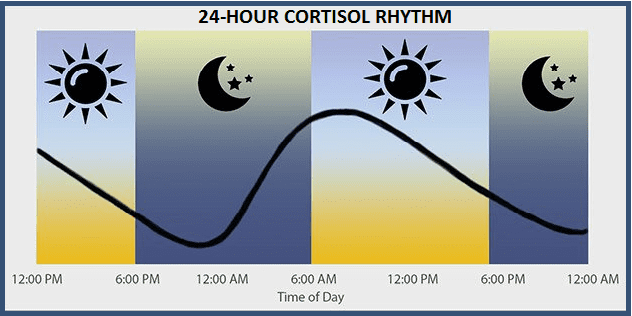
In addition to its secretion in response to any stress, cortisol levels also follow a regular 24-hour (circadian) rhythm and its measurements throughout the day and in the evening are the key indicators of HPA axis function (Fries et al., 2009).
The figure below depicts a typical 24-hour rhythm for salivary cortisol. Its levels are highest in the morning and then fall for the rest of the day and evening.
Researchers have shown that abnormal circadian patterns of ‘free’ salivary cortisol levels through the course of the day correlate with various sub-clinical or symptomatic and disease conditions including type 2 diabetes, metabolic syndrome, clinical depression, chronic fatigue syndrome, persistent pain, and cardiovascular disease (Chrousos, 2009).
The saliva cortisol test results are shown as a similar graph in the actual test results.
Overview of cortisol measurement methods
Whether stress is acute or chronic, physical, emotional or environmental, it affects the levels of cortisol secreted throughout 24 hours. There are three main methods of measuring cortisol levels using:
- Saliva
- Blood (serum/plasma)
- Urine
Most studies of conditions with altered HPA axis activity rely on determining ‘free’ cortisol production over the course of a day using the most credible methods supported by scientific literature, and focus on either multiple samplings of saliva or 24 hour urine collection.
At present saliva is the most commonly used sample specimen to measure cortisol levels (at least by functional medicine practitioners, if not conventional doctors). It’s considered the most biologically relevant specimen type used to assess cortisol concentrations compared to other specimen types such as serum and urine samples, since only ‘free’, non-protein bound and biologically relevant cortisol measures are analysed in saliva at a given point of time.
As cortisol is predominantly bound to the cortisol binding protein, the unbound fraction is considered more readily available to the cell of the body. It’s this free hormone that best reflects a patient’s hormone-related symptoms, rather than total or bound hormone levels as measured in serum.
Importantly, the 24-hour cortisol rhythm is also mapped out when using saliva cortisol test. It’s also the easiest and most convenient test to perform as all samples can be collected at home and send to the lab at your convenience.
Serum/ plasma measurements reflect total cortisol (when collected over 24 hours) and are usually taken at one point during the day (most commonly in the morning during blood collection for a blood test), as collecting multiple samples during the day can be difficult to do as well as stressful for most individuals.
Around 90% to 95% of circulating cortisol in blood/plasma is bound to proteins which makes it unavailable for biological activity (Hellhammer et al., 2009). Thus total ‘free’ cortisol can’t be measured in blood.
However, blood cortisol tests (in addition to the saliva cortisol test) can be useful when assessing significant, life altering adrenal dysfunctions such as the Cushing syndrome and Addison’s disease (see more on it below).
24 hour fresh urine test can measure total and ‘free’ cortisol which represent a total free cortisol production over the course of a day; however, it is unable to chart the circadian variations of cortisol excretion at certain times of the day.
Hair cortisol can also be used to assess chronic stress by capturing extended exposure to elevated levels of cortisol (Levine et al., 2007).
Recently, a new method of assessing cortisol levels was developed using four samples of dried urine to provide 24-hour cortisol assessment (the DUTCH test). However, compared to the extensively researched saliva test, there is no peer reviewed publication to date (as far as I am aware) that has verified the methodology used or how the data obtained from dried urine compares to saliva or serum.
I look forward to learning more about the DUTCH test by reading research studies when they are published. In the meantime, I’ll keep utilising the saliva cortisol test that proved to be of great help in my clinical practice.
The table below summarises and compares the features of saliva, hair, fresh urine, and blood, and their usefulness in cortisol measurements as described in the scientific literature.
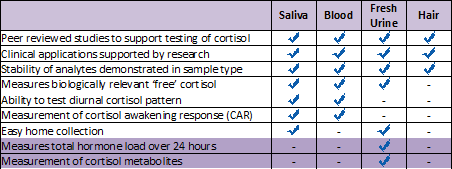
Source: Salimetrics
Other HPA axis dysfunctions: Cushing syndrome and Addison’s disease
Since cortisol plays a key role in regulating multiple systems in the body, it’s a very tightly regulated hormone. As mentioned above, about 90 to 95% of circulating cortisol in plasma is found bound to proteins and is not used for biological functions.
Excess amounts of circulating ‘free’ cortisol can lead to adrenal insufficiency conditions such as Cushing’s syndrome. The incidence of Cushing’s syndrome, caused by prolonged use of glucocorticoid therapy or to adrenal tumours, is very low and reported to be at approximately 0.7 to 2.4 individuals per million in the general population (Newell-Price et al., 2006).
Another condition with very low levels of circulating cortisol is known as Addison’s disease where the adrenal glands produce inadequate levels of cortisol. The incidence of Addison’s disease is approximated at 40-140 individuals per million people (Newell-Price et al., 2006).
Both Cushing’s syndrome and Addison’s disease are at the extreme ends of the spectrum of cortisol level excretion and not frequently observed in practice. On the other hand sub-clinical manifestations of HPA axis dysfunctions, such as adrenal fatigue/ burnout quite commonly impact our health and wellbeing nowadays.
Summary
Saliva adrenal hormones test is easy to do at home, non-invasive and it accurately determines the 24-hour cortisol rhythm by collecting four saliva samples through the course of the day to determine salivary cortisol levels at certain times.
It’s a scientifically credible method of evaluating cortisol levels. There are hundreds if not thousands scientific publications in peer reviewed literature supporting and validating its use and providing both credible and useful information on cortisol.
Using saliva, cortisol rhythm measurements are stress-free, straightforward and have better compliance. The results reflect the free, bio-available hormone levels, unlike blood which measures total levels.
That’s why I’ve been using the saliva adrenal hormones test for adrenal fatigue assessment, it also is a pretty accurate treatment guide initially, as well as when re-testing further along the treatment to check how well it’s progressing.
Please note that all information provided in this post is intended as a guide only and is not aimed to be an in-depth look at all cortisol testing methods available at present. It represents my clinical experience when helping clients with adrenal fatigue recovery, and is also based on the available scientific research – I’ve included some of the articles and/or studies I looked at in the references below.
Contact me to select the most appropriate evaluation method for your circumstances, given your current health status and requirements.
What’s your experience or view on adrenal hormones testing methods? Have you done the saliva adrenal hormones test yourself?
Comment below if you agree or disagree with what’s discussed in this post. Let’s debate the pros and cons of each method!
Good health and blessings
Joanna Sochan
Wholistic Health and Lifestyle Therapist
Natural and Lifestyle Solutions for Abundant Health & Wellbeing
Photos credit: Pixabay
References
- Salimetrics – https://www.salimetrics.com/
- Chrousos, G.P (2009). Stress and disorders of the stress system. Nat Rev Endocrinol, 5, 374-381.
- Fries, E., Dettenborn, L., and Kirschbaum, C (2009). The cortisol awakening response (CAR): facts and future directions. Int J Psychophysiol, 72, 67-73.
- Hellhammer, D.H., Wust, S., and Kudielka, B.M (2009). Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology, 34, 163-171.
- Levine, A., Zagoory-Sharon, O., Feldman, R., Lewis, J.G., and Weller, A (2007). Measuring cortisol in human psychobiological studies. Physiology & behavior, 90, 43-53.
- Newell-Price, J., Bertagna, X., Grossman, A.B., and Nieman, L.K (2006). Cushing’s syndrome. Lancet, 367, 1605-1617.
- Ryan, R., Booth, S., Spathis, A., Mollart, S., and Clow, A (2016). Use of Salivary Diurnal Cortisol as an Outcome Measure in Randomised Controlled Trials: a Systematic Review. Ann Behav Med, 50, 210-236.
- Thorn, L., Hucklebridge, F., Evans, P., and Clow, A (2006). Suspected non-adherence and weekend versus week day differences in the awakening cortisol response. Psychoneuroendocrinology , 31, 1009-1018.
- Woods, D.L., and Mentes, J.C (2011). Spit: saliva in nursing research, uses and methodological considerations in older adults. Biological research for nursing, 13, 320-327.
Additional resources
- Adrenal fatigue, sleep and cortisol connection
- Holy basil – a key herb for stress, anxiety, depression and fatigue
- Magnesium for anxiety, stress, high blood pressure and muscle pain
- Low blood pressure – how to raise it naturally
- Top nutrition tips for insomnia and interrupted sleep
Disclaimer: The above material is for informational and/or educational purposes only. It should not be used to self-diagnose and it is not a substitute for a medical advice, diagnosis, treatment, prescription or recommendation. All viewers of this content, especially those taking prescription or over-the-counter medications, should not make any changes in their health regimen or diet before first consulting a doctor or other qualified health provider with any questions they may have regarding a medical condition or their particular circumstances.

Joanna Sochan is a Natural Therapist and founder of Naturimedica Holistic Health & Wellness. She has a passion for helping her clients transform their lives by becoming healthy and well naturally. Joanna is a fatigue, sleep and gut health expert helping tired, stressed or unwell individuals to regain their energy, sleep better and be happier, more relaxed and calm. Joanna practices in Sydney and Lake Macquarie, Australia and also conducts online consultations for clients Australia-wide. View full bio.
 Print This Post
Print This Post 

Leave A Comment